- 01865317483, 07856131431
- help@gbclinics.co.uk
Shoulder Pain Conditions
- Home
- Shoulder Pain Conditions
Frozen Shoulder
What Is Frozen Shoulder?
Frozen shoulder, medically known as adhesive capsulitis, is a condition that causes pain, stiffness, and loss of movement in the shoulder joint. It typically develops gradually and can last for months or even years if left untreated.
This condition occurs when the capsule surrounding the shoulder joint becomes inflamed and thickened, forming adhesions that restrict movement.
Who Gets Frozen Shoulder?
Frozen shoulder most commonly affects people aged 40 to 60, and is more common in women. Risk factors include:
- Diabetes
- Thyroid disorders
- Previous shoulder injury or surgery
- Prolonged shoulder immobilisation
- Cardiovascular disease
Symptoms of Frozen Shoulder
- Frozen shoulder progresses in three main phases:
- Freezing Phase (6 weeks to 6 months)
- Gradual onset of shoulder pain
- Increasing stiffness
- Pain worsens at night and with movement
-
- Frozen Phase (4 to 12 months)
-
- Pain may reduce, but stiffness remains severe
- Daily activities like dressing, reaching, or driving become difficult
-
- Thawing Phase (6 months to 2 years)
-
- Range of motion slowly begins to improve
- Full recovery may take time, and some stiffness may persist
Diagnosis
At our clinic, frozen shoulder is diagnosed through:
- A thorough clinical assessment of shoulder mobility and function
- Diagnostic ultrasound scanning to rule out other causes of shoulder pain (e.g., rotator cuff tears or bursitis)
Treatment Options
Early and appropriate treatment can significantly reduce recovery time and improve your quality of life. We offer a range of non-surgical treatments including:
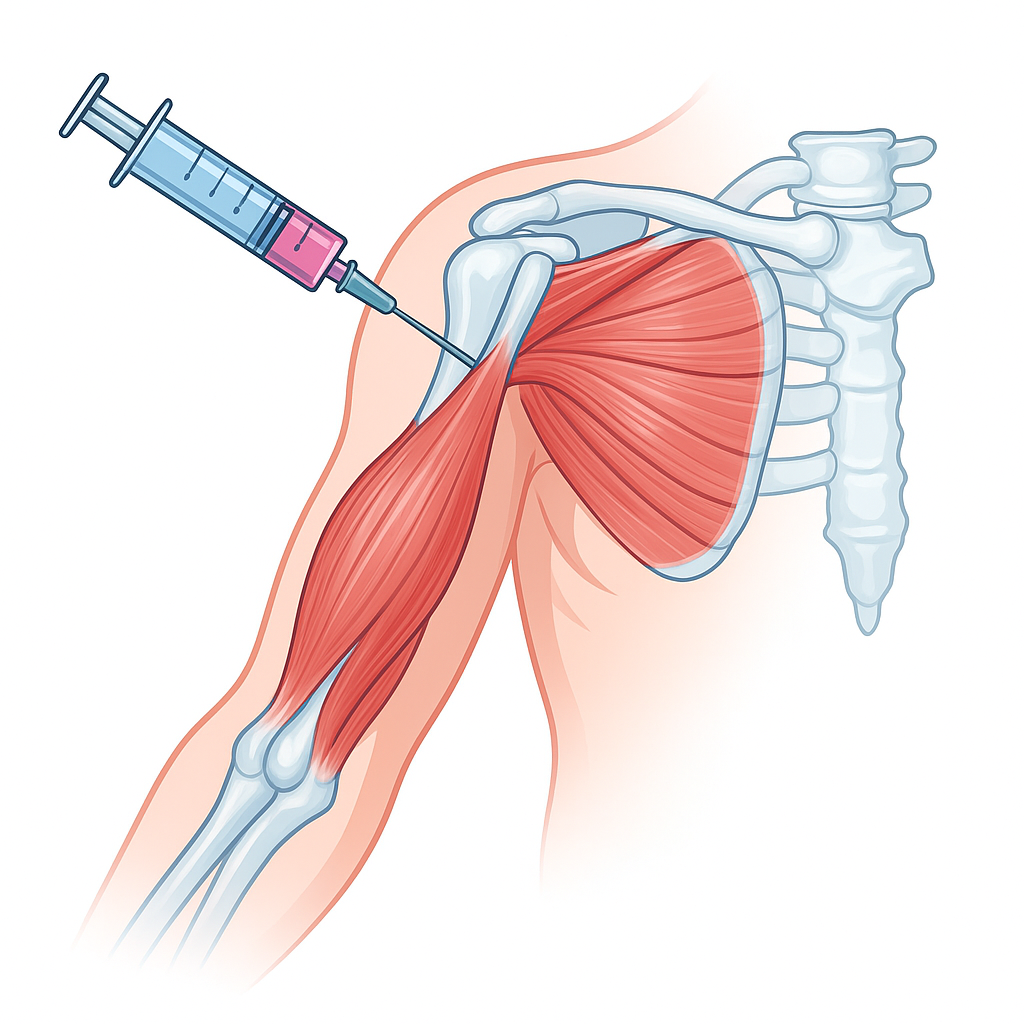
Corticosteroid Injections
Steroid injections reduce inflammation inside the shoulder joint capsule, helping to:
- Relieve pain
- Improve sleep
- Enable better participation in physiotherapy
Benefits:
Hydrodistension (Hydrodilatation)
Also known as capsular distension, this is an advanced treatment option for moderate to severe frozen shoulder.
What is it?
Hydrodistension involves injecting a sterile fluid mixture (saline, corticosteroid, and local anaesthetic) into the shoulder joint capsule to:
- Stretch and expand the tight joint capsule
- Break down adhesions
- Reduce pain and improve range of motion
Procedure Details:
- Performed under ultrasound guidance
- Local anaesthetic ensures comfort during the procedure
- Takes about 20–30 minutes
- Most patients can return home shortly after
Physiotherapy: The Key to Full Recovery
Physiotherapy plays a crucial role in the treatment and long-term recovery of frozen shoulder. Whether you’ve had an injection, hydrodistension, or are managing the condition conservatively, physiotherapy helps to:
- Restore shoulder flexibility and strength
- Improve joint function
- Prevent long-term stiffness
- Support each stage of recovery with tailored exercises and manual therapy
Your personalised rehab plan may include:
- Passive stretching and mobilisations
- Range of motion and strengthening exercises
- Postural correction and movement education
- Gradual return-to-activity programme
Rotator cuff and subacromial pain syndrome
Subacromial Pain Syndrome & Rotator Cuff Disorders
What You Need to Know
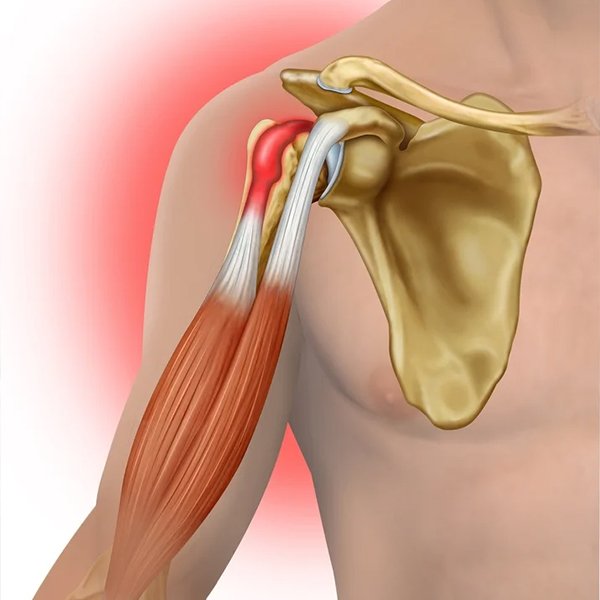
Shoulder pain is one of the most common musculoskeletal complaints, and a large proportion of it originates from the subacromial space—a narrow area between the top of the shoulder blade (acromion) and the rotator cuff tendons. This is often referred to as Subacromial Pain Syndrome (SAPS), which includes a range of conditions involving irritation, inflammation, or damage to the rotator cuff.
What Is Subacromial Pain Syndrome?
Subacromial Pain Syndrome is a broad term used to describe shoulder pain arising from structures in the subacromial space. This often includes:
- Rotator cuff tendinopathy or tears
- Subacromial bursitis
- Impingement of soft tissues beneath the acromion
- Degenerative changes or inflammation from overuse or poor mechanics
Understanding the Rotator Cuff
The rotator cuff is a group of four muscles and tendons that stabilise the shoulder and help lift and rotate the arm. These tendons can become irritated or torn due to overuse, poor posture, repetitive overhead activity, or trauma.
Common Rotator Cuff Disorders Include:
- Tendinopathy: Degeneration or inflammation of the tendons
- Partial or Full-Thickness Tears: Ranging from mild damage to complete rupture
- Subacromial Bursitis: Inflammation of the fluid-filled sac that cushions the tendons
- Calcific Tendinitis: Calcium deposits forming within the tendon, causing pain and inflammation
Symptoms to Watch For
- Pain on the outside or front of the shoulder
- Discomfort with lifting, reaching overhead, or sleeping on the affected side
- Weakness when raising or rotating the arm
- Clicking or catching sensation during movement
- Limited range of motion
Accurate Diagnosis Is Key
At our clinic, we provide a comprehensive shoulder assessment, ensuring accurate diagnosis and efficient treatment planning:
- Clinical examination of movement, strength, posture, and impingement signs
- Diagnostic musculoskeletal ultrasound scan to visualise the rotator cuff tendons, bursa, and subacromial space in real time
- Referral for MRI if deeper imaging is necessary for complex or full-thickness tears
Treatment Options at Our Clinic
We offer a full range of non-surgical, evidence-based treatments tailored to your diagnosis and lifestyle:
Physiotherapy
- Targeted strengthening and mobility exercises
- Postural re-education
- Manual therapy techniques
- Gradual return-to-activity programmes
Ultrasound-Guided Injections
- Corticosteroid injections to reduce inflammation in the subacromial bursa and relieve pain
- Performed under real-time ultrasound guidance for precise targeting and effectiveness
Shockwave Therapy (if available)
- Stimulates healing in chronic tendon conditions such as rotator cuff tendinopathy or calcific tendinitis
Referral to Specialist
For significant rotator cuff tears, persistent pain, or failed conservative treatment, we facilitate referral to an orthopaedic consultant for surgical consideration
Why Choose Us?
Same-day assessment, diagnosis, and treatment Expert-led care by a Consultant Physiotherapist with over 20 years’ experience
Diagnostic ultrasound and injections performed in-clinic
Fully registered with HCPC and CSP
Personalised rehabilitation to help you recover faster and avoid recurrence
Don’t Let Shoulder Pain Hold You Back
Subacromial pain and rotator cuff disorders are treatable—and early intervention makes a big difference. Whether your pain is new or long-standing, we’re here to help you move better, feel stronger, and return to the activities you love.
Book your consultation today and take the first step toward a pain-free shoulder.
Understanding Shoulder Arthritis and How We Can Help
Calcific Tendonitis & Barbotage Treatment
Effective Relief from Shoulder Pain with Advanced Ultrasound-Guided Therapy
What Is Calcific Tendonitis?
Calcific tendonitis is a condition where calcium deposits form within the tendons of the rotator cuff, most commonly in the shoulder. These deposits can cause intense pain, inflammation, and limited movement, particularly during flare-ups.
It often affects people aged 30 to 60 and can develop without a clear cause, although repetitive strain, poor biomechanics, and age-related changes may contribute.
Common Symptoms
- Sudden or gradually worsening pain in the front or top of the shoulder
- Sharp pain when lifting the arm or lying on the affected side
- Stiffness and reduced range of motion
- Night pain, often disturbing sleep
- Tenderness over the rotator cuff tendons
How Is Calcific Tendonitis Diagnosed?
At our clinic, we use diagnostic musculoskeletal ultrasound to:
- Detect and measure the calcium deposits
- Assess inflammation or associated bursitis
- Evaluate tendon health in real-time during movement
This quick, non-invasive scan gives a clear and immediate diagnosis.
What Is Barbotage?
Barbotage (also called ultrasound-guided needling or lavage) is a minimally invasive procedure used to break down and remove calcium deposits from the tendon. It is considered the gold standard for treating calcific tendonitis when conservative treatments fail.
How Barbotage Works
Performed under real-time ultrasound guidance, the procedure involves:
- Using a fine needle to puncture the calcium deposit
- Washing it out with sterile saline solution to break down and flush out the calcium
- Injecting local anaesthetic and, if needed, a corticosteroid into the bursa to reduce post-procedure inflammation
The entire procedure is usually completed within 30–45 minutes and does not require general anaesthesia or hospital admission.
Benefits of Barbotage
Immediate pain relief in many cases Minimally invasive
Performed in-clinic under local anaesthetic Reduces the need for surgery Accelerates return to normal activities Ultrasound-guided for maximum accuracy and safety
What to Expect After the Procedure
- Mild discomfort for 24–48 hours (can be managed with over-the-counter pain relief)
- Gradual improvement over several days to weeks
- Follow-up physiotherapy is often recommended to restore strength and mobility
Why Choose Us for Barbotage?
Start Your Recovery Today
If you’re suffering from shoulder pain due to calcific tendonitis, Barbotage offers a fast, effective, and non-surgical solution.
Book your consultation today to get an expert assessment and access to cutting-edge treatment—right in our clinic.
Glenohumeral joint / shoulder joint Osteoarthritis
What Is Glenohumeral Joint Osteoarthritis?
Glenohumeral osteoarthritis is a degenerative condition affecting the main shoulder joint—where the upper arm bone (humerus) meets the shoulder socket (glenoid). Over time, the cartilage that cushions the joint wears away, leading to pain, stiffness, and reduced mobility.
This condition is most common in adults over the age of 50, but it can also develop earlier due to injury, repetitive stress, or previous shoulder surgery.
Common Symptoms
Patients with glenohumeral osteoarthritis often experience:
- Deep, aching pain in the shoulder
- Stiffness, especially in the morning or after rest
- Difficulty lifting the arm or reaching overhead
- Clicking, grinding, or catching sensations during movement
- Muscle weakness around the shoulder
- Pain that worsens with activity and improves with rest
What Causes It?
Glenohumeral osteoarthritis can develop due to:
- Age-related wear and tear
- Previous shoulder injuries (dislocations, fractures)
- Repetitive use or heavy lifting over many years
- Inflammatory conditions such as rheumatoid arthritis
- Genetic predisposition or joint abnormalities
How Is It Diagnosed?
At our clinic, we use a combination of clinical expertise and advanced imaging to accurately diagnose shoulder arthritis:
- Comprehensive shoulder assessment: To evaluate your range of motion, strength, and function
- Diagnostic musculoskeletal ultrasound: To assess joint inflammation, bone changes, and surrounding soft tissues in real time
- Referral for X-rays or MRI if further joint detail is needed
Treatment Options We Offer
Our clinic offers a full range of non-surgical treatments aimed at reducing pain, improving mobility, and delaying or avoiding surgery:
Physiotherapy
- Tailored exercises to improve flexibility, strength, and joint support
- Manual therapy techniques to improve joint mechanics
- Postural training to reduce shoulder strain during daily activities
Ultrasound-Guided Injections
- Corticosteroid injections to reduce inflammation and relieve pain
- Hyaluronic acid injections (e.g., Ostenil®, Durolane®, to lubricate the joint and improve movement
- All injections are performed under ultrasound guidance for maximum precision and effectiveness
Referral to Orthopaedic Specialist
If conservative treatment doesn’t provide sufficient relief, we can refer you to an orthopaedic consultant for further options, including joint replacement.
Why Choose Our Clinic?
Same-day assessment, imaging, and treatment Expert care by a Consultant Physiotherapist with over 20 years’ experience Use of diagnostic ultrasound and ultrasound-guided injections Fully registered with the Health & Care Professions Council (HCPC) and Chartered Society of Physiotherapy (CSP) Personalised, evidence-based care plans
Take the First Step Toward Relief
Shoulder arthritis can make daily life difficult—but help is available. Early diagnosis and treatment can help you manage symptoms, avoid surgery, and keep doing the things you love.
Contact us today to book your consultation and start your journey to a pain-free shoulder.
Long head of the Biceps tendon
Understanding Biceps Tendon Disorders: Causes, Symptoms & Treatment
The biceps muscle plays a key role in the strength and stability of your upper arm and shoulder. When problems arise in the biceps tendon—such as inflammation, degeneration, or tearing—they can significantly impact your ability to lift, carry, or even perform everyday tasks.
What Are Biceps Tendon Disorders?
Biceps tendon disorders involve damage or irritation to one or both tendons that connect the biceps muscle to the shoulder and elbow. The most affected is the long head of the biceps tendon, which travels through the shoulder joint.
-
Common Biceps Tendon Conditions
-
1
Biceps Tendonitis
Inflammation of the tendon, often due to overuse, repetitive overhead activity, or age-related wear and tear. -
2
Tendinosis
Chronic degeneration of the tendon tissue, typically without significant inflammation—often seen in people over 40. -
3
Tendon Tears or Ruptures
Partial or full tearing of the tendon, which can occur suddenly due to lifting or trauma, or gradually from degeneration. -
4
Superior Labrum Anterior to Posterior (SLAP) Tears
Involves injury to the labrum (cartilage) where the biceps tendon anchors in the shoulder.
- Symptoms to Watch For
- Pain in the front of the shoulder or upper arm
- Weakness with lifting or rotation of the arm
- Clicking or popping sensation in the shoulder
- Tenderness along the biceps tendon
- A noticeable bulge in the upper arm (in cases of tendon rupture – “Popeye muscle”)
Diagnosis: How We Assess Biceps Tendon Injuries
At our clinic, we use a comprehensive assessment to identify the specific cause of your pain. This includes:
- Clinical examination: Checking for tenderness, strength loss, and movement limitation
- Diagnostic musculoskeletal ultrasound: Real-time imaging to detect inflammation, degeneration, or tears in the tendon
- Additional referrals for MRI or orthopaedic consultation if more complex shoulder involvement is suspected
Treatment Options at Our Clinic
We offer a range of advanced, evidence-based treatments tailored to the severity of your condition:
-
Physiotherapy
Targeted rehabilitation including stretching, strengthening, and postural correction to reduce strain on the tendon and restore function. -
Ultrasound-Guided Injections
- Corticosteroid Injections: For inflammation and acute pain relief
- Hyaluronic Acid or combination injections: For chronic tendinopathy and joint lubrication
- Performed under ultrasound guidance to ensure accurate, safe delivery of medication
- Regenerative therapy like shockwave therapy, prolotherapy, PRF -
Shockwave Therapy (if available)
A non-invasive treatment that promotes tendon healing in chronic conditions. -
Referral to Orthopaedic Specialist
For tendon ruptures or complex shoulder injuries that may require surgical repair.
Don’t Ignore Biceps Tendon Pain
Early treatment can prevent minor irritation from progressing into more serious damage. Whether you’re dealing with a sports injury, work-related overuse, or age-related degeneration, we can help you recover faster and avoid long-term issues.
Book Your Assessment Today
If you’re experiencing shoulder or upper arm pain, contact us for a same-day consultation and diagnostic ultrasound scan. Get the right diagnosis and start your recovery today.
Understanding Acromioclavicular (AC) Joint Disorders: Causes, Symptoms & Treatment Options
Shoulder pain can come from several different structures, but one commonly overlooked source is the acromioclavicular (AC) joint—the small joint where the collarbone (clavicle) meets the top of the shoulder blade (acromion). Though small, this joint plays a vital role in shoulder movement and stability, especially during overhead or cross-body actions.
What Is the AC Joint?
The AC joint is located at the top of the shoulder. It allows for subtle gliding movements and helps transfer loads between the arm and the rest of the skeleton. Despite its size, it is a common site of pain and dysfunction, particularly in active individuals, manual workers, and older adults.
Common AC Joint Disorders
- AC Joint Osteoarthritis
- Degeneration of the joint cartilage due to age, repetitive use, or prior injury
- Common in people over 40 or those who frequently lift or perform overhead activities
- AC Joint Sprain or Separation
- Often results from a fall directly onto the shoulder or trauma
- Severity ranges from mild ligament sprain to complete dislocation of the joint
- AC Joint Inflammation (Synovitis or Capsulitis)
- Can develop from repetitive stress or following an acute injury
- Causes pain, swelling, and restricted shoulder movement
- Symptoms of AC Joint Disorders
- Pain at the top of the shoulder, especially when pressing on the joint
- Discomfort during overhead, cross-body, or heavy lifting movements
- Swelling or a visible bump at the joint
- Clicking or grinding sensation with movement
- Limited range of motion or stiffness in the shoulder
Diagnosis: Accurate, Timely, and Non-Invasive
At our clinic, we provide same-day diagnosis using:
- Detailed clinical assessment to evaluate joint stability, pain triggers, and shoulder mechanics
- Diagnostic musculoskeletal ultrasound, which can detect inflammation, fluid buildup, joint degeneration, or ligament injury
- Referral for X-ray or MRI if deeper structural imaging is required
Get Expert Help Today
If you’re struggling with pain at the top of your shoulder, we’re here to help. Our expert team offers same-day assessment, diagnostic ultrasound, and image-guided treatment—all in one visit.
Book your consultation today and take the first step toward pain-free movement.
Treatment Options We Offer
- We take a targeted, evidence-based approach to help relieve your AC joint symptoms and restore shoulder function:
🔹 Physiotherapy- Strengthening exercises to stabilise the shoulder
- Manual therapy and posture correction
- Activity modification to reduce joint stress
🔹 Ultrasound-Guided Injections
- Corticosteroid injections to reduce inflammation and pain
- Performed under real-time ultrasound guidance for precise, safe delivery directly into the AC joint
🔹 Hyaluronic Acid Injections (For degenerative AC joint arthritis)
- Improves lubrication and joint movement
- Ideal for patients who want to delay or avoid surgery
🔹 Referral to Orthopaedic Specialist
- For severe separations or persistent pain that doesn’t improve with conservative care
Why Early Treatment Matters
AC joint disorders, if left untreated, can lead to chronic pain, weakness, and reduced function of the shoulder. With timely intervention, most conditions can be managed effectively without surgery.
Regenerative Therapy & Medicine for Shoulder Conditions at GB Clinics
At GB Clinics, we offer cutting-edge regenerative therapies designed to help you overcome shoulder pain and improve mobility. Whether you’re dealing with rotator cuff injuries, arthritis, tendonitis, or any other shoulder condition, our regenerative medicine treatments are tailored to stimulate healing, reduce pain, and restore function without the need for surgery.
Regenerative therapies are designed to promote natural healing by enhancing the body’s ability to regenerate damaged tissues. By utilizing Platelet-Rich Fibrin (PRF), shockwave therapy, and Prolotherapy, we help repair and rejuvenate the shoulder tissues, reduce inflammation, and get you back to your daily activities.
How Can Regenerative Therapy Help Shoulder Conditions?
Shoulder conditions like rotator cuff injuries, tendonitis, frozen shoulder, and shoulder arthritis can significantly impact your ability to move and perform everyday tasks. Regenerative therapies are becoming an increasingly popular option because they offer non-invasive solutions with minimal downtime, providing effective relief for both acute and chronic conditions.
Here’s how regenerative therapies at GB Clinics can help:
- Stimulate Tissue Healing: By using your body’s own natural healing mechanisms, we promote the regeneration of damaged tissues in the shoulder, helping you heal faster.
- Reduce Pain and Inflammation: Our treatments target the root cause of your pain and reduce inflammation, which is often the source of discomfort in shoulder conditions.
- Improve Function: Regenerative therapies help restore flexibility, strength, and range of motion, which can be hindered by injuries or degeneration in the shoulder.
- Avoid Surgery: Regenerative treatments offer an alternative to surgery, allowing you to heal without the risks and recovery time associated with more invasive procedures.
Our Regenerative Treatments for Shoulder Conditions
At GB Clinics, we offer a combination of advanced treatments to provide you with a comprehensive, personalized solution for your shoulder condition.
How It Helps Shoulder Conditions:
- Repairs Rotator Cuff Injuries: By promoting collagen production and repairing damaged tendons and ligaments.
- Reduces Tendonitis Symptoms: Helps alleviate pain and restore function to tendons.
- Aids in Arthritis Relief: Reduces inflammation and encourages cartilage repair, helping to slow the progression of arthritis.
- Platelet-Rich Fibrin (PRF) Therapy
What It Is: PRF with a higher concentration of fibrin, a protein that helps tissue healing. It has a slower release of growth factors, allowing for longer-lasting healing.
How It Helps Shoulder Conditions:
- Enhances Healing of Soft Tissues: By promoting more effective tissue regeneration in the shoulder.
- Reduces Pain and Swelling: Helps control inflammation while supporting collagen production.
- Improves Joint Health: Particularly beneficial for arthritic conditions in the shoulder.
Best For: Chronic shoulder pain, tendon and ligament injuries, and arthritis.
- Shockwave Therapy
What It Is: Shockwave therapy uses high-energy sound waves to stimulate healing in the damaged tissues. The waves promote blood flow, reduce pain, and trigger cellular repair mechanisms in the affected area.
How It Helps Shoulder Conditions:
- Stimulates Tissue Regeneration: Enhances the healing process of damaged tendons and muscles.
- Reduces Pain and Muscle Tightness: Effective in treating shoulder impingement, tendonitis, and frozen shoulder.
- Improves Mobility: Helps to break down scar tissue and reduce stiffness, making movement easier and less painful.
Best For: Tendonitis, frozen shoulder, rotator cuff injuries, and chronic shoulder pain.
- Prolotherapy
What It Is: Prolotherapy is an injection-based treatment that involves injecting a mild irritant into the damaged tissues of the shoulder. This stimulates the body to repair the injured area by promoting collagen production and tissue regeneration.
How It Helps Shoulder Conditions:
- Strengthens Ligaments and Tendons: Helps restore stability to the shoulder joint.
- Repairs Soft Tissue Damage: Encourages natural healing and repair of ligaments and tendons, particularly beneficial for long-standing injuries.
- Reduces Chronic Pain: Addresses the root cause of pain by regenerating tissues and reducing inflammation.
Best For: Rotator cuff injuries, chronic tendon injuries, shoulder instability, and ligament tears.
Why Choose GB Clinics for Regenerative Therapy?
At GB Clinics, we offer a personalized and holistic approach to treating shoulder conditions. Our experienced team of physiotherapists and specialists works closely with you to determine the best course of treatment based on your specific needs. Here’s why our clinic is the ideal choice for your shoulder recovery:
- Expert Care: Our team consists of highly trained professionals who specialize in regenerative medicine and musculoskeletal conditions.
- Comprehensive Treatments: We offer a range of regenerative therapies like PRF, shockwave therapy, and prolotherapy, ensuring we provide the most effective treatment for your condition.
- Non-Surgical Solutions: We focus on non-invasive treatments that can help you avoid the need for surgery, offering a safer and more convenient path to recovery.
- Advanced Technology: We use the latest techniques and equipment, such as ultrasound-guided injections, to ensure precision and effectiveness in your treatment.
- Tailored Recovery Plans: Your treatment plan is customized based on your condition, age, lifestyle, and goals, ensuring the best possible outcome.
Start Your Recovery Today at GB Clinics
If you’re suffering from shoulder pain or injury, regenerative therapies at GB Clinics can provide the relief and healing you need. Our expert team is here to guide you through every step of your recovery, ensuring you receive the best care and support.
Contact us today to schedule your consultation and learn more about how PRF therapy, shockwave therapy, and prolotherapy can help you recover from shoulder conditions and get back to living pain-free.